On 20th May 2019 Hugh McCaughey (@HughMcCaughey), National Improvement Director for the NHS in England led his first #Improve4Patients tweet chat. It was hosted by the NHS Horizons team (@HorizonsNHS) who also prepared this report. The tweetchat lasted for one hour from 7pm to 8pm.
These were the questions asked during the tweet chat:

What happened during the tweet chat?
777 people joined the chat (data from Followthehashtag). The tweet chat was promoted and supported by a group of 31 "Improvement superconnectors"; people active in the improvement movement in the English NHS who have broad networks of influence on social media. Their efforts attracted a large, diverse group of contributors to the tweet chat.
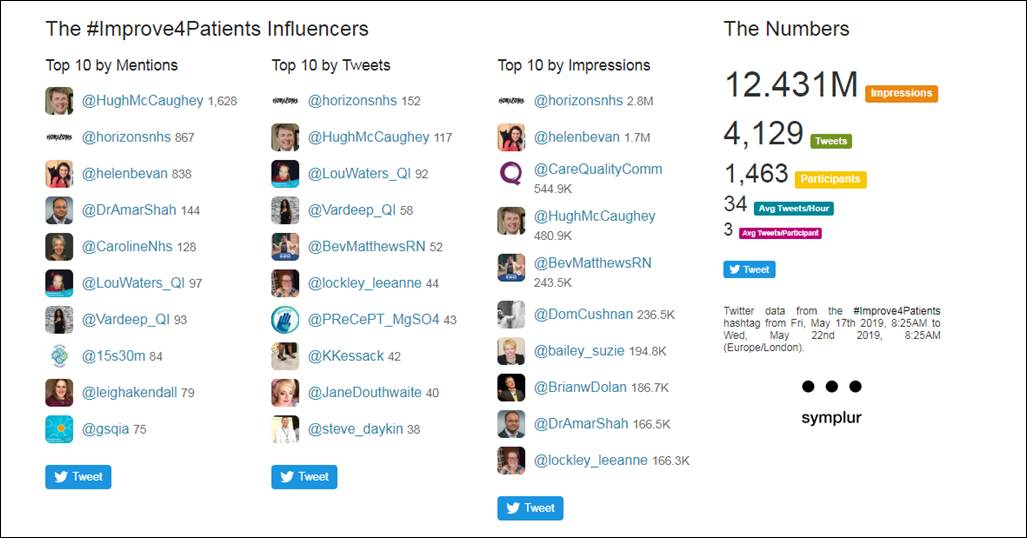
These are the tweet chat influencers as identified by the Symplur analytic platform:
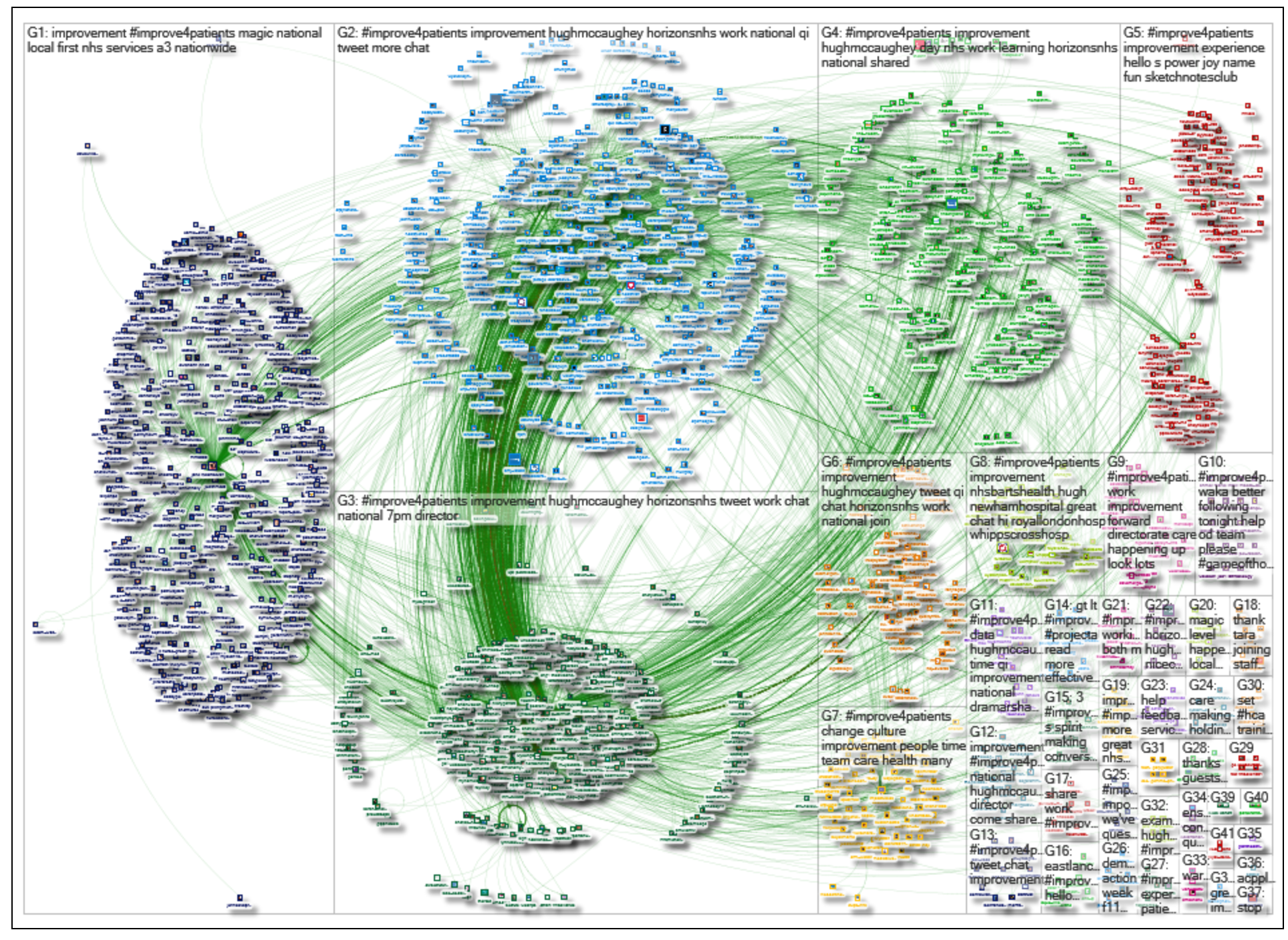
The graph below from NodeXL evidences how diverse groups of people were connected by the tweet chat. The clusters are individuals and accounts that tweet about similar issues, and the green lines show that they were connecting with one another during the tweet chat, building a strong improvement community (click here to see a larger version). Thank you to Dr Graham Mackenzie, a Scottish trainee GP, who created this graph.
We are delighted to see that people are continuing to build this community beyond the tweet chat by using the #Improve4Patients tag.
The NHS Horizons team evaluated the 1,991 tweets sent during the tweet chat (data from Symplur) and identified 49 specific ideas.
We grouped the feedback and ideas in to the following themes:
- Specific improvement ideas
- Joined-up working
- Shared purpose
- Creating conditions for improvement
- Co-production with patients
- Capacity for improvement
- Training
- Measurement for improvement
- Language
- Regulation
(Tip: To view an original tweet click on the image, click on the red text to view response tweets)
We have pulled out key tweets under each of these headings below. You can also read more of the tweets in our Twitter Moment.
Specific improvement ideas
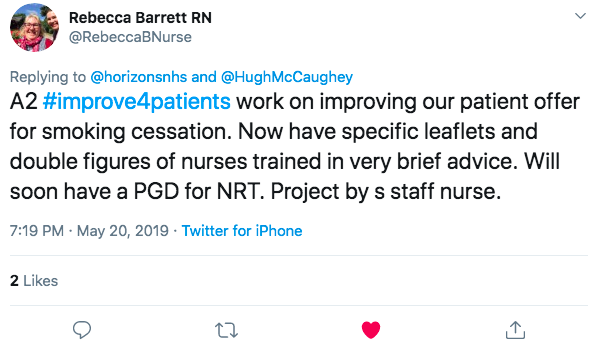
Rebecca Barrett told us about the staff nurse led project working across facilities and professions to give patients a more tailored service.

Rebecca Barrett also described the work at Nottingham to improve the patient offer for smoking cessation. They now have specific leaflets and double figures of nurses trained in very brief advice.
Andrea Hargreaves team uses graffiti boards for ideas generation and 'rocks in my shoes box' for regular idea and issue solving.

Tanya Saker shared this pressure point injury graphic from North Bristol Trust.

The @SignUpToSafety campaign was effective, said Mark Juniper: it provided focus & structure to enable local QI work.




Joined-up working
In Nottingham, they join teams up together working across an integrated care system (ICS) as Steve Daykin explained.

Suzie Bailey agreed, saying that we should help to stop reinventing approaches and evolve them instead.
Yvonne Hastings reflected that we ought to provide more platforms with similar teams across regions, to network and learn from each other.
Charlotte Fox suggested using existing infrastructure and networks that are well-established and have the ability to cultivate, capture, and disseminate good work.

 We need to invest in creating a common community and shared approach to quality improvement across public services respectful of our different contexts and local languages said William Lilley.
We need to invest in creating a common community and shared approach to quality improvement across public services respectful of our different contexts and local languages said William Lilley.
 Tim Gillatt explained that they are encouraging operational teams to visit each other through our safer collaborative. Tim said they've loved the opportunity to see what other people are doing in other hospitals and pinch with pride.
Tim Gillatt explained that they are encouraging operational teams to visit each other through our safer collaborative. Tim said they've loved the opportunity to see what other people are doing in other hospitals and pinch with pride. 
Ceri Charles agreed, saying these networking sessions often give you the precious time and space to step out of your role and connect with others
At Gloucestershire Safety & Quality Improvement Academy they ask staff to register their projects. Where there are similar projects they aim to connect teams so they are not duplicating effort. Plan-Do-Study-Act (PDSAs) are also very important so only changes that work are implemented & spread. They do this via a Google forum. Louise also said all staff doing QI through the Academy are allocated a QI facilitator for duration of their project. Collaboratives offer additional opportunity to work with wider teams. Louise echoed Helen Bevan's observation that magic happens when local teams at the point of care redesign their own services.


Jonathon Gray suggested that we should join up all Q, IHI, Health foundation and all thousands of staff; don't create new departments.




 Creating conditions for improvement
Creating conditions for improvement
Vardeep responded to say that this shows the value of relationship building when on you are journey of improvement.
Lynne Bowers shared her belief that staff and people need protected time and space, permission to attend, not being 'bleeped' out to attend to 'urgent' matters.
Leeanne Lockley had a similar reflection: to give people time to understand what’s expected of them; let them ask questions and answer them open and honestly - QI is a marathon not a sprint!
Dr Amar Shah said active sponsorship from senior leaders, access to data, support to involve service users in the work is necessary. He also wondered why there are so few chief quality officers on our boards in England.
Minesh Khashu thought a big objective should be to teach NHS boards to understand QI better. It is a weak link at present and pushes organisations to a reactionary behaviour rather than continuous improvement.
Improvement needs to be linked back to strategic objectives and overall organisational aims - consistency, always with the patient in mind reflected Lou Waters.
The senior leadership team and Board at Warrington and Halton Hospitals seeing it as a top priority and support the development of their Quality Academy, said Ursula Martin.

Vin Diwakar said that his projects have worked because of an acceptance by senior leaders that large scale change is messy and just because it doesn't follow a linear approach doesn't mean it isn't good.

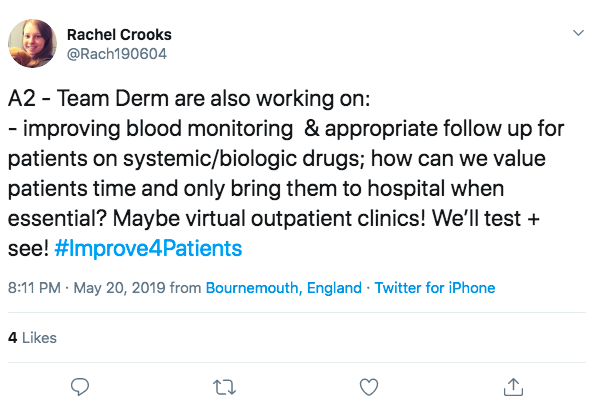
This was echoed by Rachel Crooks, who said that continuous feedback is important in the success of a project. Mentoring is crucial said Abi Byrchmore, who asked for more support when starting and finding your way through your first project.
 William Lilley said we have to spend more time understanding how to foster the local leadership behaviours that create that rarest of qualities 'psychological safety' #improve4patients that seems to make or break improvement efforts.
William Lilley said we have to spend more time understanding how to foster the local leadership behaviours that create that rarest of qualities 'psychological safety' #improve4patients that seems to make or break improvement efforts.
This was echoed by Hassan Al-Omari, who thinks its important to understand that its ok to fail so long as the lessons learned are applied to the future. We need a culture of safe exploration of QI projects.
Richard Best suggested having a little space with a team to examine purpose, allowing them to own what they want to change, guiding them with simple steps - celebrate learning success or not.

Emma Saunders had a similar reflection: she has found that listening to front line staff and giving them permission to make the changes that are needed has been a great start. Emma says we need more of this, more transparency, more two way communication and more opportunity to put heads together and develop ideas nationally. Emma is passionate about empowering her colleagues to find their “agency” and making real and meaningful change happen at a grassroots level as she described in this tweet.
Hugh McCaughey said we should be seeking to empower the hundreds of thousands of front line staff who want to make their services better.

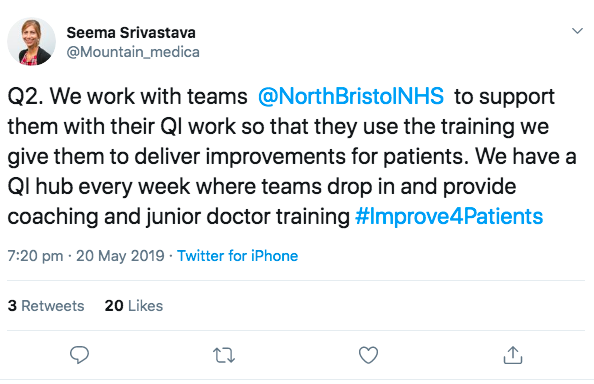
The East England Ambulance Service explained that it's important to encourage improvement ideas from all grades and levels of staff from your office admin through the chief exec! A lot of answers/suggestions come from their crew rooms. Similarly Steve Daykin agreed with this; he said the project leads does not have to be and should not always be the team leaders and service managers. They can be and should be frontline staff being nearest the change ideas.
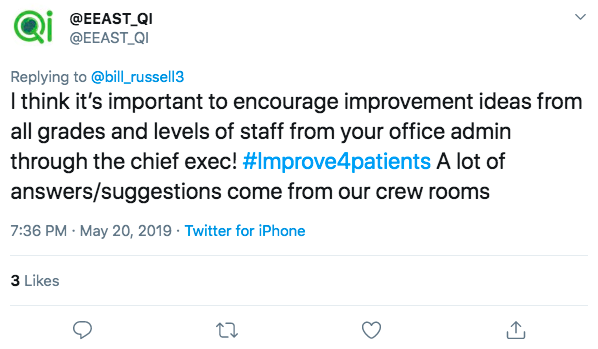
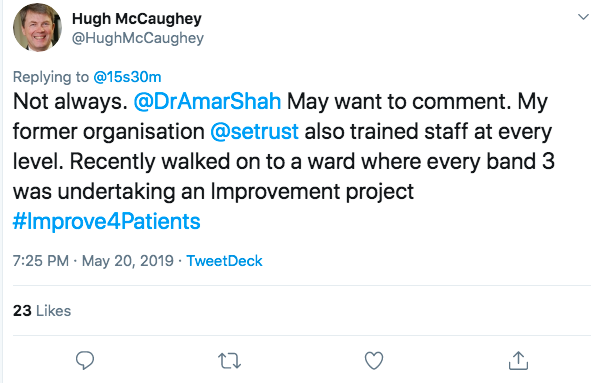
Hugh McCaughey said his former organisation South East Trust also trained staff at every level. He recently walked on to a ward where every staff member working at band 3 was undertaking an improvement project.

Rebecca Barrett suggested shared governance empowers nurses to attempt to change things for the better. There are hundreds of staff actively looking to make improvements for patients. Supported centrally, given training, opportunities to write up and share practice wider.

Compassionate culture is essential, said Sally Brown. Staff need to feel restored and supported to improve - they cannot change/improve from an empty cup. Stressed and burned out staff have no head space for improvement or compassionate care. Invest in well being, tackling stress and burnout.
Great wisdom from Caroline Poole, who summed up much of the sentiment in the tweet chat: Coaching not telling. Learning not failing. Measuring not guessing. Team not solo. Appreciating strengths not searching for failings. Celebrating success. Being visible. Shared power. Oh, and as much fun, laughter, joy as possible.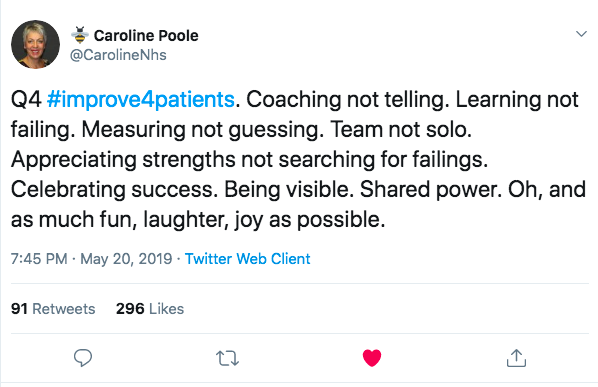
Jane Douthwaite felt it is important we move beyond consultation and co production with improvements and let users and staff at the point of care co design solutions, test, implement & evaluate.
Steve McCue agreed it's all about relationships, and "integration moves at the speed of trust".
This sentiment was echoed by Sue Holden, who reminded us that we need to remember improvement happens with through and by people; by Sarah Cooper, who reflected that collaboration, conversations, relationships, and thinking of how this will impact care for our citizens is needed; and by Sameena, who said "When there is trust, then people seem to go with the fails and the wins. When things go wrong and people can still look at the positive lessons - that feels great!" Sound data, strong relationships with teams, collaborative working, interdisciplinary work, celebrating success was a contribution from The Centre from Sustainable Healthcare. Tom Downes had a similar description of what has been important to his improvement work.
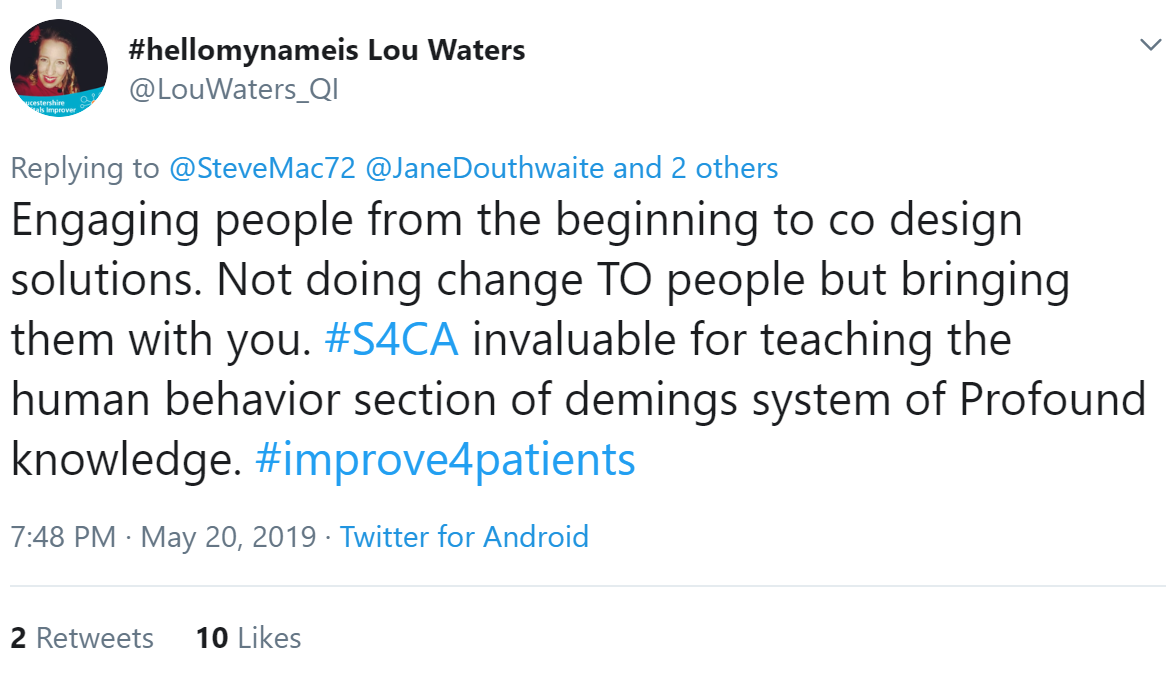
Lou Waters summed it up, saying it's important to engage people from the beginning to co design solutions. Not doing change TO people, but bringing them with you.
Elaine Latham reinforced this: celebrate success, share challenges, keep the messages (purpose) alive to build momentum but keep it real. Above all be authentic.
East England Ambulance service also shared they are visiting ambulance stations around the Trust and putting on Quality Improvement cafes and giving people the chance to drop in and have a chat about improvement. They also invite their stakeholders and publish regular updates via newsletters. The same service also shared that they use ‘virtual crew rooms’ to engage with our staff via Facebook.

Co-production with patients
We must ask the patients and staff on frontline what matters to them. If they own the issue they will come up with the solution using QI methods said Farzana Hussain. 
This view was supported by Claire Shields who said patient choice is key in encouraging improvement; Lynnette Lee who expressed the importance of asking people who will be affected or benefit from change; by Steve McCue, who reflected that we must consider the wider determinants of health and how we collaborate better with patients; and by Sally Brown, who said involving people (patients, families carers) is absolutely essential.

Nicola had a similar reflection: she said too much is driven by those with no lived experience/direct knowledge.
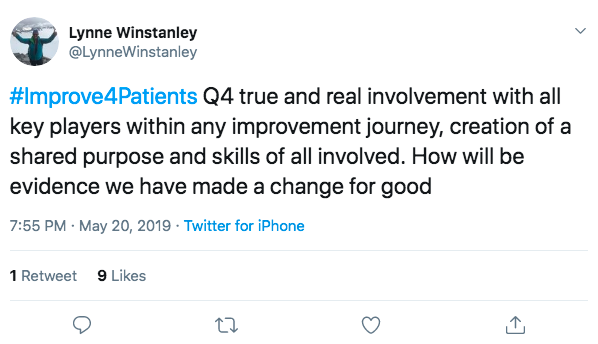
Lynne Winstanley asked the important question: How do we strengthen involvement in #QI from the real people who use our services how do we really co-design with our true customers?
Elaine Latham said in the South West patients and public trained in QI meet with improvers as part of a panel discussion.

Paul Conroy echoed this sentiment: "It's time to see patients & carers as part of the team delivering and improving care".
Matthew Mezey suggested we encourage the spread of coproduced 'Always Events' around the UK - to guarantee patients can always give positive reports when they've received excellent care.

There is good practice with co-production, as Jennifer Poll described:
 Co-design has helped PReCePT communicate effectively with their users.
Co-design has helped PReCePT communicate effectively with their users. 
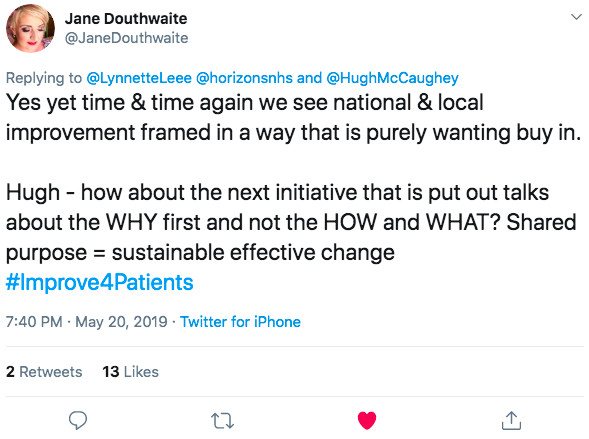
Shared purpose
Jane suggested the next initiative that is put out talks about the WHY first and not the HOW and WHAT? Shared purpose = sustainable effective change.
Alice O'Neil agreed: the shared purpose is the 'reason why', the driver and connection across all. Lynnette Lee also explained the importance of shared purpose.
Caroline Poole added we can achieve collaborative strength when there's shared purpose.
The first question is not "what is our aim?" (although that's an important question) but "who are our people?" said Helen Bevan.
Supporting staff in sharing their work in easily accessible ways, ensuring everyone knows 'why' at patient level, demonstrating measurable impact and celebrating results - appreciation and thanks goes a long way, shared Robert Ayers.
Steve Daykin reflected that to succeed with an initiative we must keep things simple, the training we deliver is not mandatory and staff contact us to get on the training, a dynamic and enthusiastic QI team build from within the existing clinical staffing with an autonomous approach.
Seeing seeing sustainable improvements for patients while empowering staff to make supported changes and where things don't go well, share it are important elements for Chris Richmond.
Elaine Latham said involvement can be at any level as long as it’s meaningful and valued. The lean management system at Medway ensures they have a consistent message to align their staff behind as a ‘line of sight’ to establish a strong support across the trust said Nick Chambers. They have trained more than 100 staff in yellow belt, and 200 in white belt.
The lean management system at Medway ensures they have a consistent message to align their staff behind as a ‘line of sight’ to establish a strong support across the trust said Nick Chambers. They have trained more than 100 staff in yellow belt, and 200 in white belt.
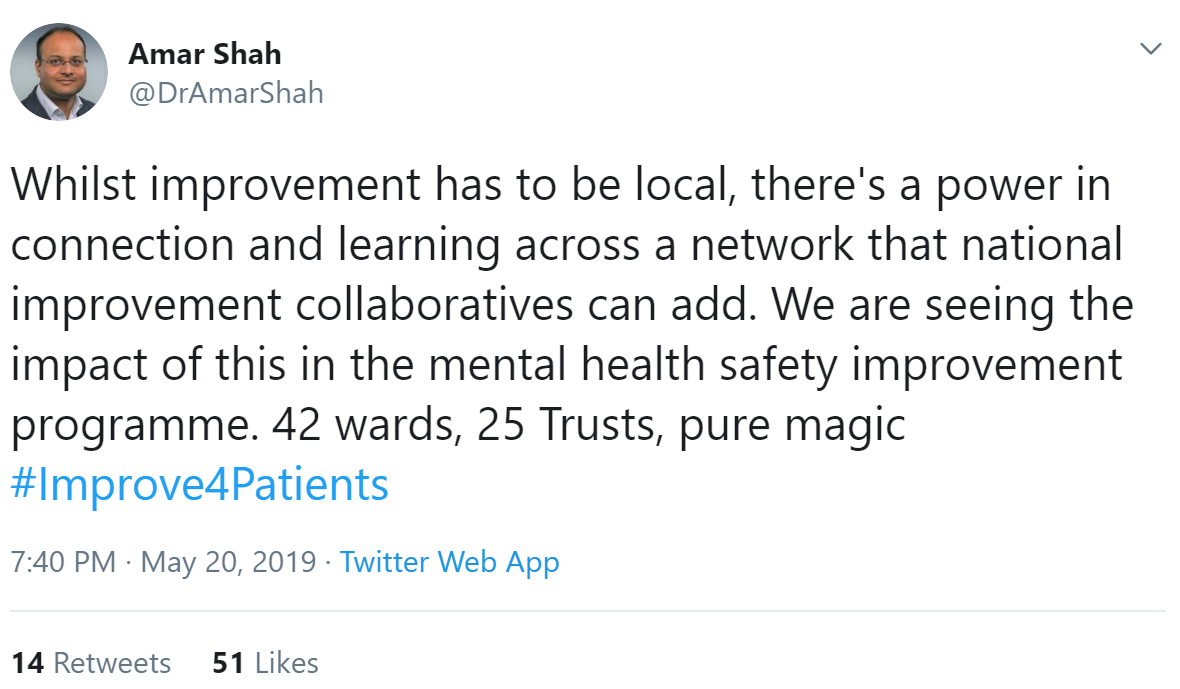
Capacity for improvement
We need a system level idea of capability and capacity to affect change at scale and pace, said Minesh Khashu.
 William Lilley is working with Billions Institute to develop the capacity and capabilities of #NHS leaders to be confident at leading large scale spread and adaption of innovations across their communities and local systems.
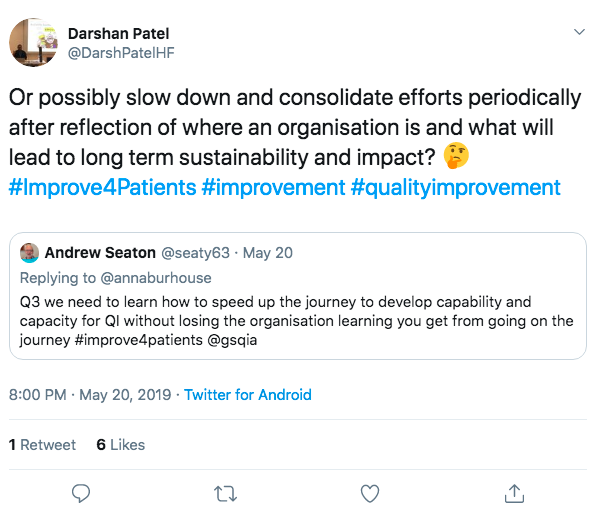
William Lilley is working with Billions Institute to develop the capacity and capabilities of #NHS leaders to be confident at leading large scale spread and adaption of innovations across their communities and local systems. Andrew Seaton said we need to learn how to speed up the journey to develop capability and capacity for QI without losing the organisation learning you get from going on the journey.
Andrew Seaton said we need to learn how to speed up the journey to develop capability and capacity for QI without losing the organisation learning you get from going on the journey.
Amanda reflected that at a national and regional level there should be an understanding of and support for the longer-term, incremental approach to improvement rather than a focus on immediate turnaround of difficult problems.

Training
Amar Shah said at East London Foundation Trust service users & carers have been part of all of their training for years. People to be supported to be meaningfully involved in improvement.
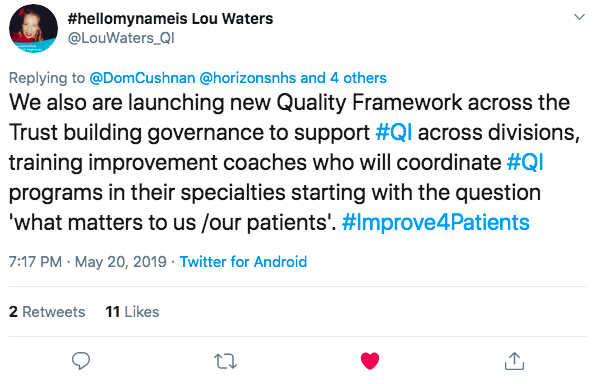
In Gloucestershire, they are launching a new quality framework building governance to support #QI across divisions, training improvement coaches who will coordinate #QI programs in their specialties starting with the question 'what matters to us /our patients'.
Charlotte Fox has been working with local universities around the implementation science that needs factoring into any improvement.
Sarah Cooper asked whether there is something about undergrad training this is where the QI journey starts for most but are the links made and embedded so it becomes business as usual and not the role of specific individuals?
In response Karen Fechter described how Health Education England has recently launched a pre-registration framework supporting leadership development & quality improvement skills in all healthcare prof undergrad curricula.
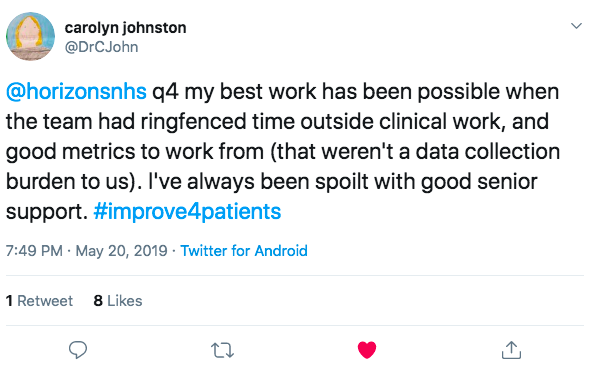
Carolyn Johnston is producing a QI guide for specific projects in anaesthesia, matching the curriculum and college clinical guidelines to suggested QI activities.
Measurement for improvement
Chris Green is helping systems across the NHS understand, and use, meaningful information and provide analysis / modelling tools to support improvement.



Language

Caroline suggested using plain English rather than technical words to be more inclusive.

Pete Gordon shared this Einstein quote.

In response Rosanna Hunt asked, do different audiences require different messages, in your experience - or does one simple headliner, or "elevator pitch" do the job well enough?
Regulation
Sasha Karakusevic said nationally we need to create the environment for individuals, organisations and systems to prosper. That’s about framing, coaching, sharing and fostering.
 Amanda agreed, stating,the hardest part is defining what the ideal will look like and then how to meaningfully measure that easily and in a way that is visually simple so everyone can see and review .
Amanda agreed, stating,the hardest part is defining what the ideal will look like and then how to meaningfully measure that easily and in a way that is visually simple so everyone can see and review .Richard Best shared that we need a serious think about blending 'branded' approaches and get back to building capability of teams to be inspired and capable of measured change. We need to start understanding why regulation has not always inspired building of capability for improvement.

Dr Joy Furnival responded to this in agreement that it would be a great idea to look at the evidence and explanations as to how regulation would further the building of improvement capability and why it has thus far been challenging. To read her research on this topic click here.
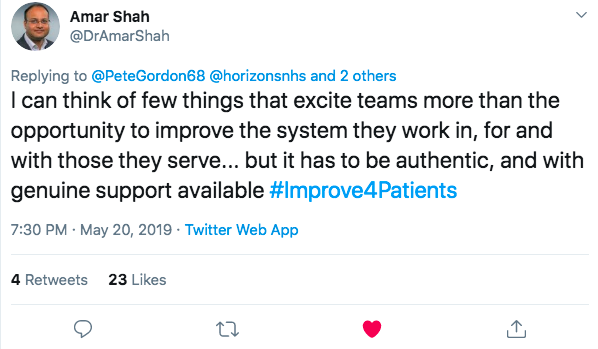
Amar Shah said he can think of few things that excite teams more than the opportunity to improve the system they work in, for and with those they serve... but it has to be authentic, and with genuine support available
Thank you for reading the report of the first tweet chat!
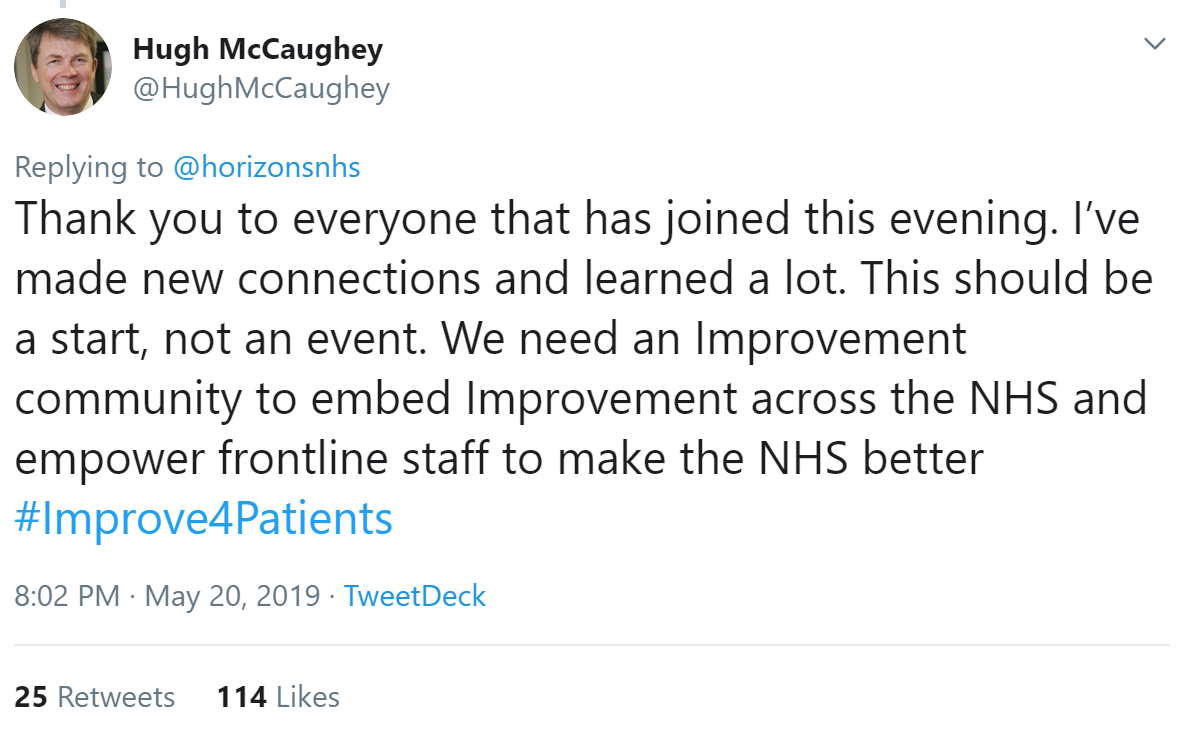
Hugh said:
We hope to see you at the next two chats:













/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-04-14-15-27-52-040-62583d78f636e9115805b2d5.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-08-05-09-59-36-465-62ecea08f636e906acfed639.jpg)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-28-14-57-17-405-62e2a3cdf636e9180c9835cb.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-20-10-16-56-533-62d7d618f636ea07987f6668.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-15-09-55-32-858-62d13994f636ea1398e71aa9.jpg)