What can we do to improve how people in the NHS work in teams?
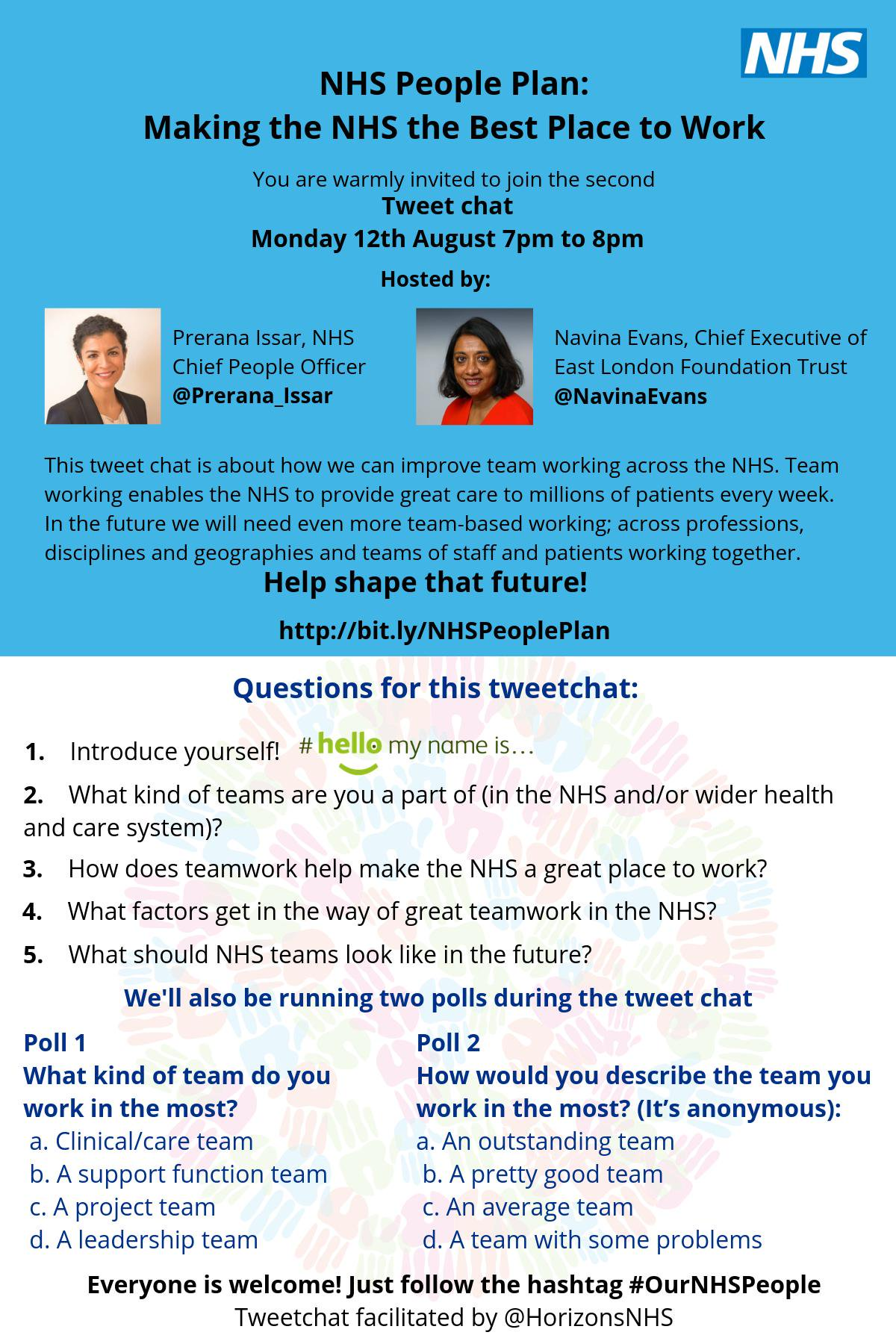
This report describes the outputs and outcomes from the NHS: Best Place to Work tweet chat that happened between 7pm and 8pm on 12th August 2019.
A tweet chat is a scheduled, organised conversation on Twitter focused around a specific topic. Anyone can join in a tweet chat, using the designated tweet chat hashtag, in this case #OurNHSPeople.
This report is written in the spirit of the tweet chat. So, for instance, we have included hyperlinks to the Twitter accounts of all the people we mention in the report. Click on the hyperlink (the red text) to go to the Twitter account of the person named or to the tweet they sent.
The tweetchat was led by Prerana Issar (NHS Chief People Officer) and Navina Evans (Chief Executive of the East London Foundation Trust, and Chair of the Best Place to Work workstream) It was facilitated by the NHS Horizons team (@HorizonsNHS) who also prepared this report. The tweet chat lasted for one hour, although the conversation continued actively on Twitter for a whole week.
These were the questions asked during the tweet chat:
What happened during the tweet chat?
The core statistics for the tweet chat are as follows:
By the time that the tweet chat finished at 8pm on 12th August, 1918 individuals had taken part.
The conversation continued on Twitter:
4,450 tweets were sent as part of the tweet chat
The reach of the tweet chat was 5,488,398. This is a count of the unique Twitter accounts that received a tweet about #OurNHSPeople. It represents the size of the audience for our tweet chat conversation. (sources of statistics: Symplur healthcare hashtags and Tweet Binder analytics).
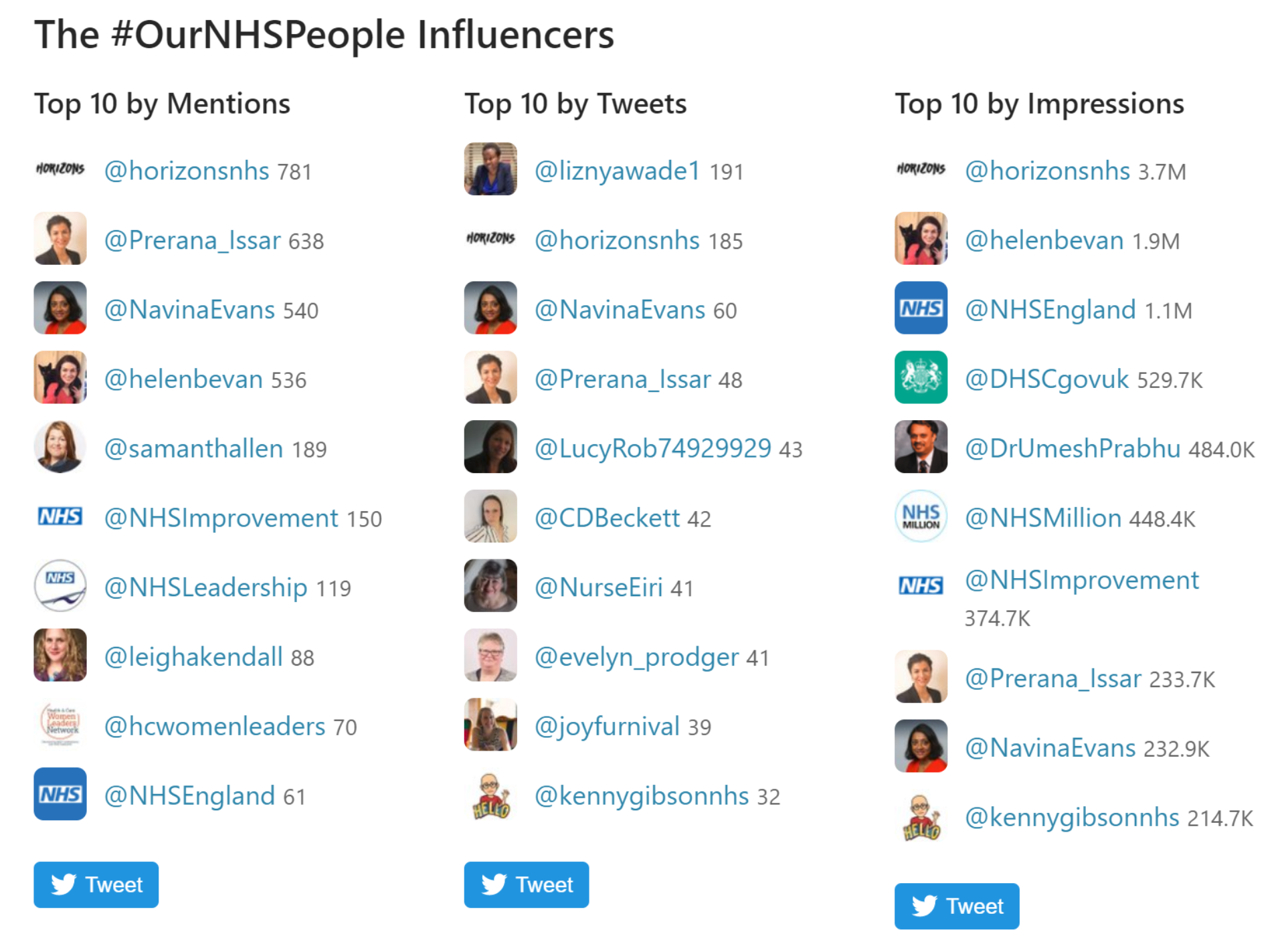
The picture below shows the leading influencers from the tweet chat. The column on the left – “top 10 by mentions” – is of interest, because these are the individuals and organisations that were mentioned by other people most often in their tweets. The second column – “top 10 by tweets” shows who took part in the tweet chat most actively. This shows a wide range of people from across the NHS.
Themes
The hundreds of people who took part in the tweet chat stated that they typically didn’t work in a team as we traditionally recognise. That is, a group of people from the same specialty and/or profession working as an entity within a defined organisational structure, working together over a long period of time. Rather, people in the NHS work in multiple teams that are constantly changing and evolving. They are teaming. This is a term coined by Amy C. Edmonson. Teaming means to collaborate across boundaries, transcending specialties and professions. It happens when challenges call upon people to collaborate with people from other specialties, departments, or organisations, especially when specific expertise is required.
We can see from the answers to question 2 (What kind of teams are you part of (in the NHS and/or wider health and care system?)) that people work in multiple teams. These teams include multi-disciplinary clinical teams; clinical and non-clinical collaboration; and leadership across a variety of teams.
Responses to question 3: (How does teamwork make the NHS the best place to work?) show that people in the NHS understand that success for themselves and for their patients is founded in collaboration including a diverse skills mix.
Factors that get in the way of great teamwork in the NHS, as revealed in answers to question 4, include silo working, and a lack of trust and respect between different bands and specialties.
Participants overwhelmingly asked that NHS teams of the future be multi-disciplinary, transcending specialism and organisational boundaries, working with a high degree of flexibility (question 5).
Teaming reflects the personalising care agenda (helping people to have greater control over their own care). Interdependent teaming across specialty, department, and organisational boundaries enables health care professionals to take a holistic view over an individual’s care, rather than the current system of conditions being treated independently. Diverse interdependent services also helps to better reflect the diversity of the populations they serve. Teaming is therefore consistent with the strong sense of purpose that people talked about in the previous tweet chat.
Amy C. Edmonson identifies three components for effective teaming:
- Enabling leadership
- Interdependence and collaboration
- Individual and collective development
In an NHS context this means:
- Leadership that enables people in the NHS to work in a way that they deem appropriate to achieve collective goals through cultivating a culture of psychological safety, effective communication, with the ability to be comfortable with fluidity, complexity and uncertainty, as well as a high level of humility and self-awareness.
- Individuals having the ability to work within and beyond specialty, department, and organisational boundaries (forming ‘squads’ as their skills are required). There needs to be a recognition that working across and outside of professional and cultural norms may present challenges: individuals need to be given a level of autonomy in order for ‘teaming’ to happen successfully.
- In the context of teaming, individuals require a ‘home’ team, to foster a sense of belonging and ‘us’-ness.

It is important to recognise that participants identify themselves not only as a member of multiple physical teams across a health economy, but also virtual teams too. Social media is enabling virtual networks and communities for learning, sharing, and mutual support including diverse specialties, professions, and patients too.
The 3-step framework from McCrystal’s Team of Teams is also useful in the context of teaming. Feedback from the tweet chat shows that NHS teams of the future need to be:
- Agile – able to move quickly and with ease
- Adaptable – able to be modified easily to suit new conditions
- Resilient – able to withstand and recover from difficult events
The tweet chat process
The first question asked participants to introduce themselves. A Twitter poll ran concurrently, and asked participants what kind of team they work in the most. There was a fairly even spread between clinical/care teams; support function teams; and leadership teams.

The responses to the second question provide further detail:
Question 2 (A2): What kind of teams are you part of (in the NHS and/or wider health and care system)?
The majority of respondents work across a variety of teams. As Hugh McCaughey said, he is part of many teams which could and should be a norm - we are all part of the NHS family. As Tim Swanwick said, if we are too focused on teams, we lose the sense of community. This was echoed by Daniel Hartley who works with many teams, as well as different networks and groups.
Many participants worked in teams that crossed clinical boundaries, working together to care for patients as articulated by Hollie Hastings, who works in primary care but sees herself as part of the wider health and care team.
Poppy Brooks is part of a local cardiology team, and her work needs to extend to wider hospital and community teams. All the teams she is linked to are essential to her role.

Similarly, Marion Lynch said she is part of an NHS England local team, cross area team, clinical team, charity team and can't think of anything she is involved in that is not a team.
@BowelGirl is from a tertiary referral centre - a small team of nurses, physios and consultants backed up with a wider team of medical physicists, patient rep, research nurses, community continence nurses. Evelyn Prodger explained how she works with multiple teams including the clinical community palliative care, and day services teams. Working with a small multi-skilled team of microbiologists, from support staff to consultants, Cherie Beckett is also part of an online team.
Working as part of a multidisciplinary team, Richard Axell works with clinical scientists, urologists, radiologists, continence nurses, radiographers and healthcare assistants to deliver a Urodynamics service. Joanne Mohammed provides ward level care to people with respiratory conditions; this ties her too the larger respiratory directorate as well as other teams within her trust. While based in primary care, Teresa Graham has links to a number of different teams across the local health economy.
A number of people work across clinical and non-clinical boundaries. Alexandra Gilder works with very mixed teams within her role in the finance team, as well as in mixed groups with clinicians, operational teams and support services. Craig de Sousa works for the executive team, a HR team, a leadership team, to name a few! Stephen Sandford also works in corporate and crosses the divide to clinical. He believes that it’s vital that we build more of these bridges between clinical and non-clinical teams.
Fiona Holley works in a corporate education team across trusts and linking with local communities.
The team boundaries that are transcended include quality improvement work. Sonya Wallbank said she works for both clinical and non-clinical teams working on culture change in their organisations. Ali Aslam enjoys the flexibility of his job as it allows him to work in both clinical and non clinical programmes whilst still maintaining a link to his 'home' team.
Robert Ayers shared that he is proud to be a member of a small team at Quality First Princess Alexandra Hospital. He also has links to the Fab NHS stuff team and the BMAT Stem academy. Also a part of many teams focused on improving staff wellbeing and patient care is Lucy Roberts, and Dave Morgan.
Joy Furnival supports a number of different improvement teams, connecting them.

Hari Grewal shared that he is part of the improvement team, whose work cannot happen without collaborating and seeing teams as being part of a wider network of improvers across the trust and the NHS.

Navina Evans and Lyse Edwards lead senior leadership teams, as well as a range of related functions.
We have seen from the responses above that we have evolved from the traditional notion of discrete teams to working across boundaries
Question 3 (A3): How does teamwork help make the NHS a great place to work?
Paul Sukhu said that nothing can be achieved alone or without collaboration, teamwork with kindness added in.

In agreement, Bev Edgar said that sharing success is the best medicine. In addition, Chris Witham added that teamwork makes the NHS a great place to work by bringing together great minds with loads of ideas united around a shared purpose. We’re better when we work together. Navina Evans said teamwork is the key to success, and can’t think of any situation where it is not.
A number of quotes were used to highlight the importance of teamwork. Robert Ayers quoted Michael Jordan ‘talent wins games, but teamwork and intelligence win championships’. Claire Hogg said “As the saying goes “team work is the dream work.”
Angela Rowe summed up the conversation:
Hugh Wilkins added that at its best teamwork provides camaraderie, mutual support and joy in work. Good teams rarely just happen, they require a lot of nurturing.
Many responses reflected the five energies needed for high-performing teams/teaming:

Related to spiritual energy, the shared purpose for NHS colleagues is delivering great patient care.


On the topic of spiritual and physical energy, Craig de Sousa highlighted that teamwork is vital for the delivery of great care for patients as well as a form of encouragement for staff members.

This was reinforced by Suzanne Tewkesbury and Lucy Roberts.
Gill Drummon said teamwork gives a shared purpose or vision and if effective has positive outcomes for both staff morale and more importantly patients, as more consistent care is provided by a cohesive team.

Related to social energies, Bill Russell stated that we must create low/flat hierarchy organisation, and socialise together. Dave Morgan agreed to this saying that he has made true friends in the group he works with. The support a good team provides helps reduce stress says Sonya Wallbank.
Work is a lot more joyful and fulfilling when part of a fantastic team says Rebecca Barrett. Ade Dosunmu concurred, said there is nothing like having a team around you for challenges and victories. Sasha Karakusevic added that working in teams helps support each other to provide and improve care for patients.
On the topic of intellectual energy Jackie Gillespie added that it’s great to have different perspectives, knowledge, skills .... but needs commitment and respect from members to make it a positive experience.

Psychological energy means offering support to one another: Prerana Issar observed that teams can drain energy or give lots of energy. And it’s nice to support each other and have some laughs together. This view was shared by @miceheath who said her current laboratory are wonderfully supportive and she really appreciates them.

Niall McDermott agreed; he said it is unrealistic for large groups of people to think as a herd, so this tension needs to be managed.
Joanne Fillingham observed that diversity is key to this, helping us avoid unconscious bias and aiding us in providing care that reflects the diversity of our populations:

As we have seen in the answers to question 2, people work transcending traditional team barriers. Bill Russell’s reflection that sharing is key to teamwork relates the wider sense of ‘teaming’:

In response, Joanne Fillingham said that in order for this to happen there needs to be a culture shift where sharing, acknowledgement and respect becomes the norm.
David Roberts had a similar reflection: teamwork is about being open and honest, seeking feedback.
Crucially, multi-disciplinary working is about meeting patients’ needs, as Christiana Melam explained.

As Kerry Eldridge said, the teams should fit around the patients.
The multi-disciplinary team working is about getting the right skills mix to serve the ever-changing needs of the population, said Mihaela Buhur…and reflecting how we ALL contribute to the patient journey.

The second poll of the chat asked how people would describe the team they work in the most.

Question 4: What factors get in the way of great teamwork in the NHS?
There were a variety of factors, including:
- A lack of clarity about team purpose
- A lack of headspace and time to get together as a team
- Negative attitudes
- Lack of trust, autonomy, and psychological safety
- Focusing too much on banding rather than the contributions individuals bring
- Silo working and conflicting priorities
Claire Hogg said lack of clarity about team purpose is a factor, as is having time for teams to get together.
This was echoed by Prerana Issar, adding a lack of shared values is often a contributing factor.
Navina Evans reflected that team work can be hindered when we lose connection to our values.

The lack of time to build team connections as mentioned above by Claire Hogg is compounded by the loss of staff rooms, increasing workloads, and a lack of caring from one another, said Harriet Brown.

Time and space is needed to build teams - putting people together does not necessarily a team make, reflected Evelyn Prodger:

This was echoed by Craig de Sousa, Mihaela Bucur, and Holly Hastings, and Deborah Davis. Rebecca Barrett shared that good teams need training to become that; she's developing this for Nottingham Hospital.
These factors relate to traditional teams. Good teamworking means more than just within your own team, it means transcending organisational boundaries too (teaming).
Silos are a barrier to good team working and crucially providing safe, effective patient care:


This is compounded by a lack of trust, systems that don’t talk to each other, and conflicting priorities shared Evelyn Prodger:

Scouse Medic identified poor communication, poor attitudes and behaviours from clinicians, silo working, lack of respect from fellow health care professionals.
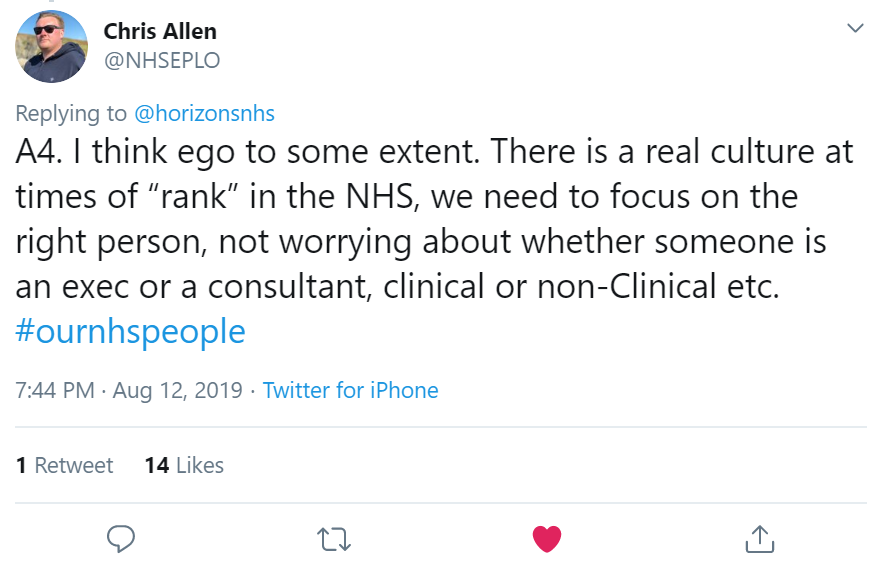
This shows a lack of respect for colleagues, seeing the band rather than the person and the value they bring.

Phil shared one-page profiles created by his organisation, Personalised Care, to build a strength-based approach.

Too many conflicting priorities can lead to silo working and pulling in different directions, rather than working together reflected Lisa Crichton-Jones .
Trust is key in any relationship, and no more so than in team working. A lack of trust in a team can cause issues, as Sherone describes:

Emma Challens cited a lack of trust and respect for each other, and a command and control structure. These are key issues that have the potential to stop effective teaming: organisations need to understand and respect what each other does.
Gaynor Walker explained that a lack of diversity and blocking inclusion gets in the way of great teamwork.


Question 5 (A5): What should NHS teams look like in the future?
An overwhelming majority of responses to this question relate to the concept of teaming; this concept is explained in more detail at the beginning of the report.
Evelyn Prodger asked that future teams be truly multi-disciplinary, not hampered by organisational boundaries:
Craig de Sousa shared this sentiment. Claire Hogg added that people need to genuinely work across patient pathways, irrespective of which organisation employs them, while Lyse Edwards said teams need to be integrated across boundaries to achieve the best for patients.
Richard Axell built on this:

Lisa Crichton-Jones asked that future teams not just be NHS:

This was echoed by Chris Witham. To do this, we need to build trust and connections across different services said Priyal Shah. Helen Bevan agreed, adding we need to start from a place of shared purpose.

As such, we need agile, responsive, multi-dimensional teams who come together when our skills are needed reflected Suzanne Tewkesbury. Ola Hill had a similar contribution.



Cherie Beckett expanded on this, saying that all roles need to be valued.

Stephen Sandford added patients, experts by experience need to be included as equals.
This was supported by Deborah Davis. Simbu agreed, and added that teams need to be able to learn from one another.



Poppy Brooks had a similar reflection. Hugh Wilkins referred to McChrystal’s Team of Teams.



The work of Brene Brown offered inspiration: Lisa Ramsey described how teams should be full of leaders – this again is related to teaming.
The final poll of the tweet chat asked for participants’ feedback:

88% of respondents finding the chat either ‘very useful’ or ‘quite useful’ demonstrates the energy and enthusiasm for the conversation about team working in the NHS.
Next steps
A further tweet chat by the best place to work workstream took place on September 9th: What do people who work in the NHS need from their leaders? The report of this tweet chat is to follow.
The first two #OurNHSPeople tweet chats has shown how much energy and interest there is in helping to make the NHS the best place to work amongst hundreds of people who work for the NHS, and for making improvements that result in a real difference to patient care.
It demonstrates the potential not just for getting the views of people on making the NHS the best place to work but mobilising them to help make it happen. These tweet chats could be the start of a social movement.



/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-04-14-15-27-52-040-62583d78f636e9115805b2d5.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-08-05-09-59-36-465-62ecea08f636e906acfed639.jpg)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-28-14-57-17-405-62e2a3cdf636e9180c9835cb.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-20-10-16-56-533-62d7d618f636ea07987f6668.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-15-09-55-32-858-62d13994f636ea1398e71aa9.jpg)