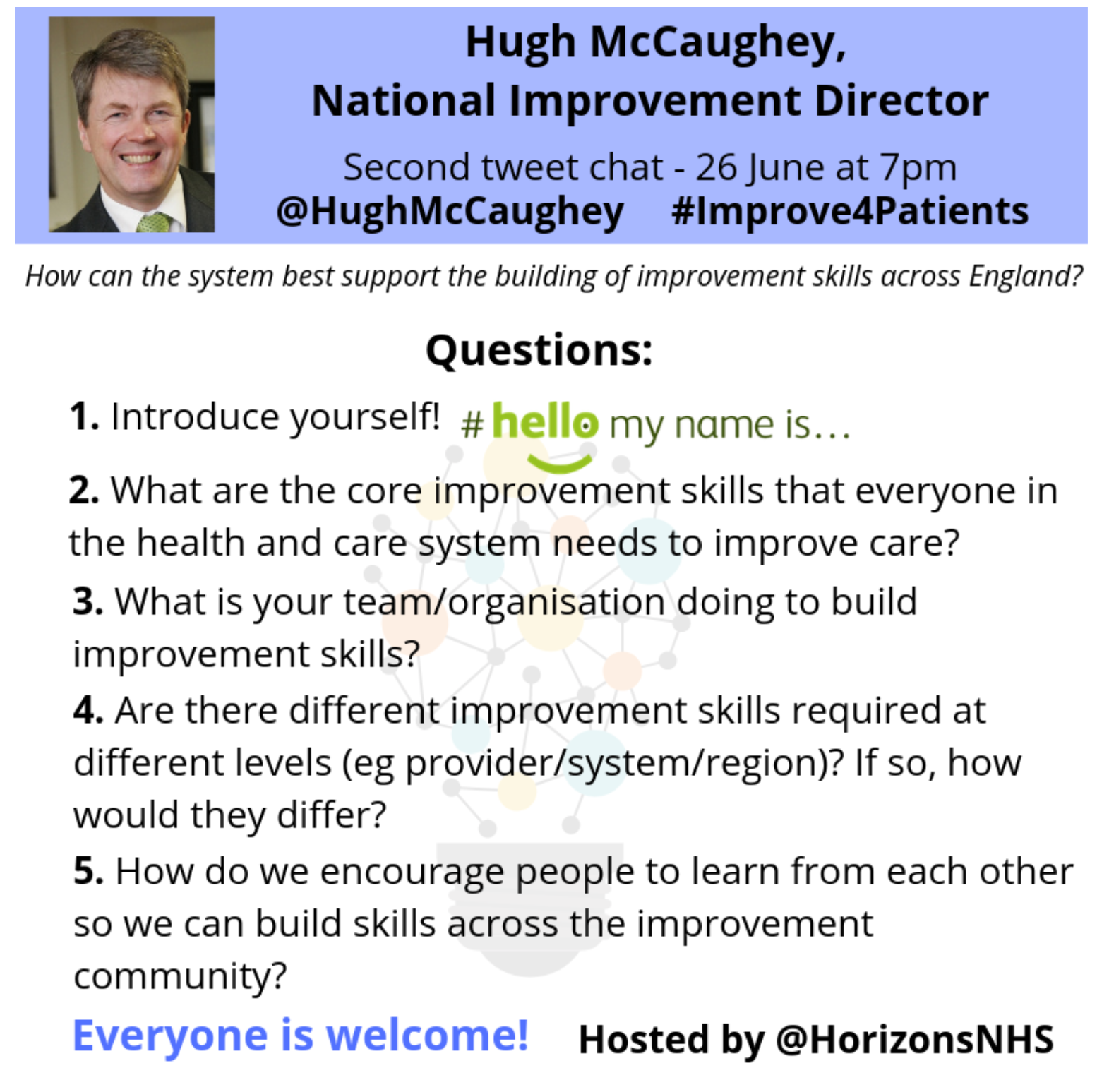
On 26th June 2019 Hugh McCaughey (@HughMcCaughey), National Improvement Director for the NHS in England led his second #Improve4Patients tweet chat. It was hosted by the NHS Horizons team (@HorizonsNHS) who also prepared this report. The tweetchat lasted for one hour from 7pm to 8pm.
These were the questions asked during the tweet chat:
What happened during the tweet chat?
There was a reach of 1.33 million (source: TweetBinder).
These are the tweet chat influencers as identified by Symplur.

The NHS Horizons team analysed the 885 original tweets (excluding retweets) sent by 549 contributors (source: Symplur and TweetBinder) grouped them in to the following themes, which include general feedback and ideas:
- Core improvement skills
- Creating conditions for improvement
- Coproduction with patients
- Leadership
- Measurement for improvement
- Tools to aid improvement
We have pulled out key tweets under each of these headings below.
(Tip: To view an original tweet click on the image, click on the red text to view response tweets)
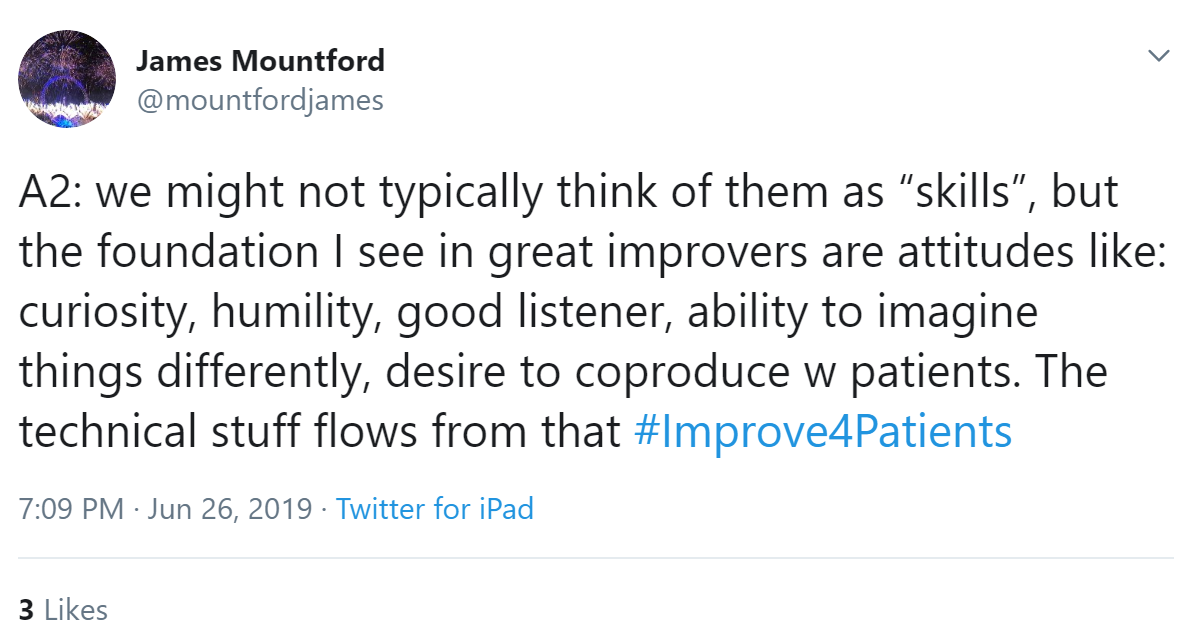
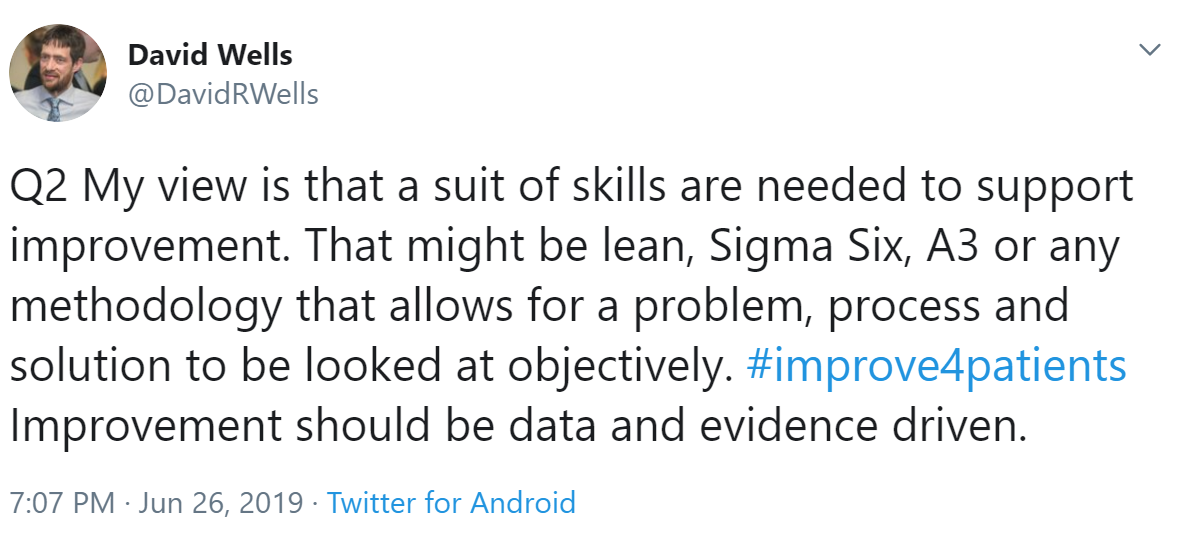
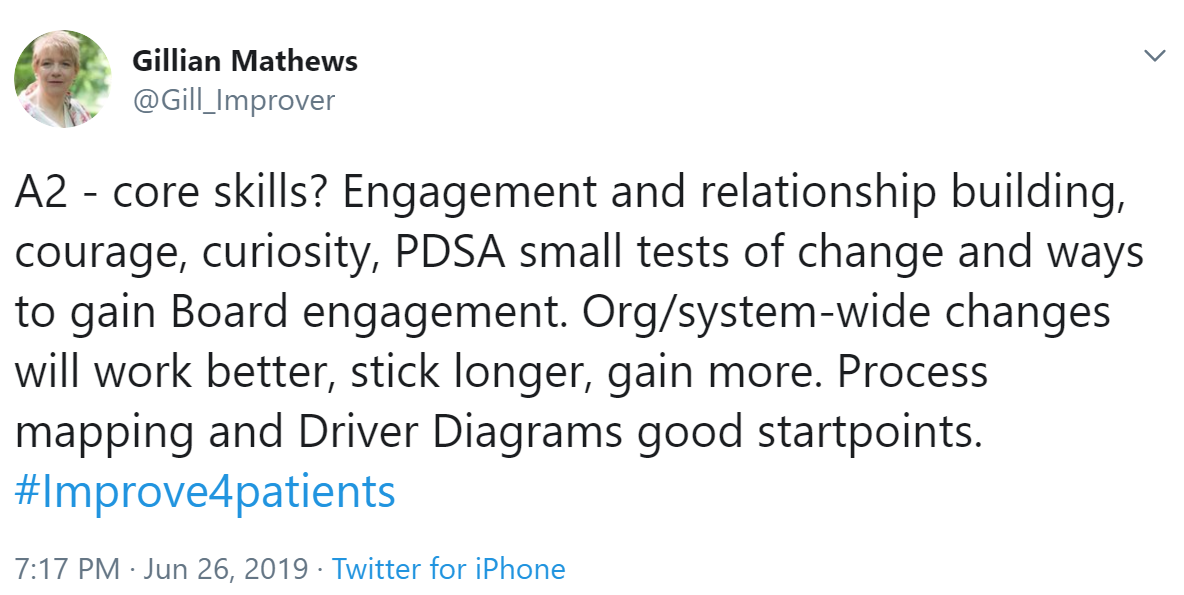
Core Improvement Skills
Lyn Williams stated that training needs to blend seamlessly into what front line staff want to do, it doesn't have to be too technical.
Joy Furnival agreed with Lyn's point, adding that sometimes core skills can be over complicated.

Kevin explained that improvement training needs to be tailored to the needs of the staff and as a result of their own ideas.

Similar to the views shared by Kevin, Binoy Perumpalath stated that staff of all levels at the organisation should be provided with improvement skills and knowledge, making it accessible for everyone.
 Embracing the uncertainty and slight fear for change is a key skill, reflected Farzana Hussain.
Embracing the uncertainty and slight fear for change is a key skill, reflected Farzana Hussain.Christopher Tuckett shared similar views to Farzana, stating that patience and persistence are important skills for QI as often things don't go to plan.
Bev Matthews shared her core improvement skills:

Leeanne highlighted that relationships are an important step to take before thinking about developing quality improvement skills.

In response, Lou Waters highlighted that as well as relationships, how to build an improvement team, who to engage, how to engage and how to design inclusively to co-produce solutions play big roles before QI is addressed.


Coaching and mentoring, awards, workshops, collaborative, webinars and different tools are things was shared by Caroline Poole.

James Frost stated that his previous trust had a team dedicated in coaching that worked across the trust.
Will Warburton shared that the Health Foundation are supporting the development of the Flow coaching academy - who help people apply the improvement methods.
The ability to book training courses online is an asset shared by Molly Kiltie.
What is your team/organisation doing to build improvement skills?

Vince Baxter's team similarly finds out what different teams would like to improve and provide them with the frameworks to implement them. Rebecca Barrett shared a similar opinion stating that we must think about how you can help others as well as how they can help you.
Within their own team, @BowelGirl says they encourage each other to re-visit ideas that have always been done in one way. Fresh eyes can definitely bring big improvements.

Hugh McCaughey replied to James; he stated that we have to make Improvement and QI accessible to all staff. It shouldn’t be exclusive. It should be like a gift to staff...enabling them to improve their jobs, their services and their outcomes for their patients
James' comment was further agreed to by James Frost who replied that the NHS rely too much on management consultants and rarely work with people on the ground.
In agreement, Bob Klaber replied that the use of technical and complicated language (sometimes very inaccessible) has not helped widen involvement beyond 'early adopters'. He suggested that accessible language would help improvement initiatives.
This also introduced the concept of dosing formula which can be read here, shared by Joy Furnival.
In addition, Caroline Poole added that there must be accessible tools and language without mystery.
Agreeing to the point above Hugh McCaughey added that we needed to make QI accessible to frontline staff without it sounding too scientific.
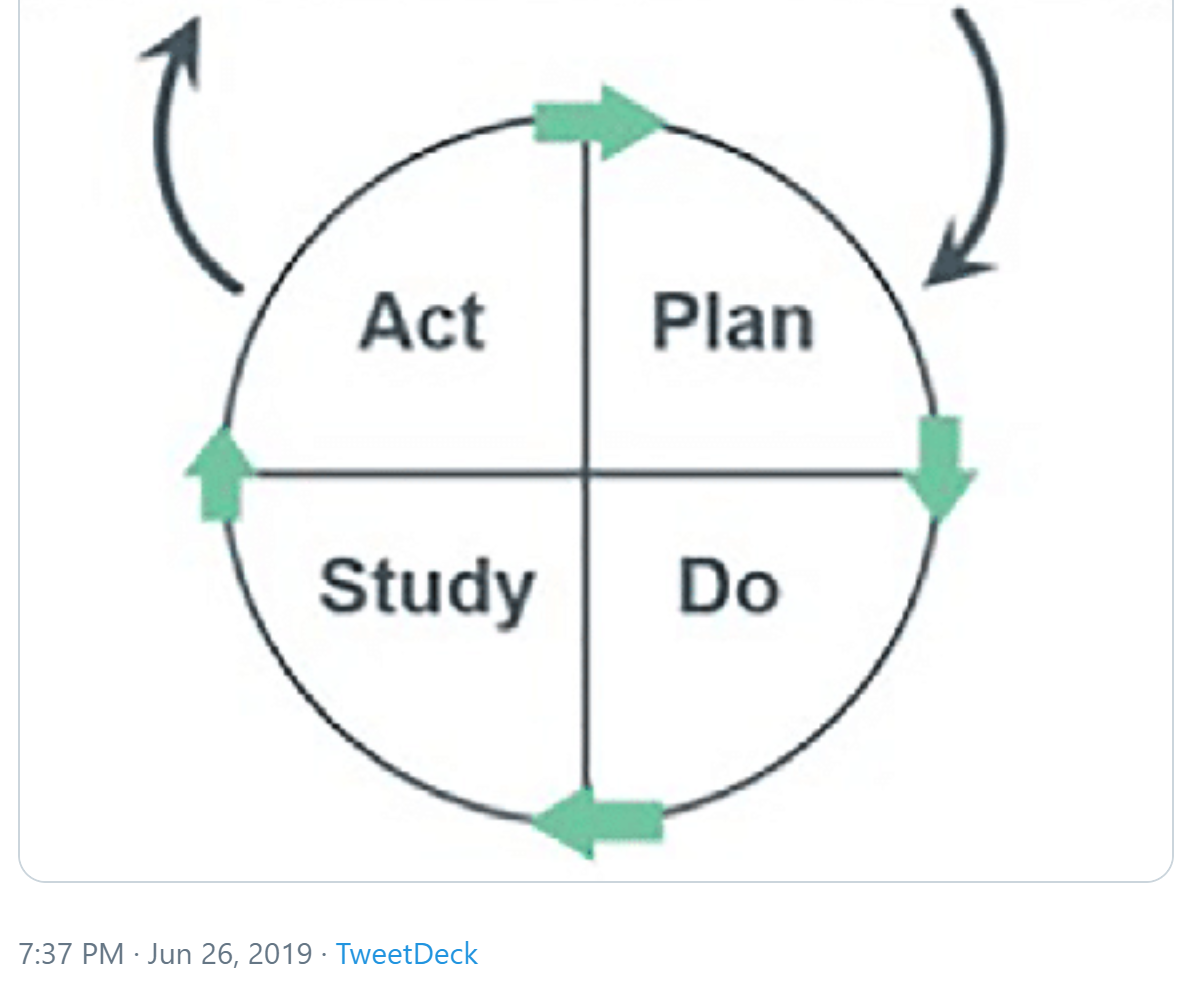
Replying to Hugh, Zoe Lord highlighted that there are many new skills, models & tools - however we shouldn’t dismiss the older ones. The model for improvement gives a much needed sense and structure to QI projects.
Suzie Bailey shared that the Berwick Review had found that not everybody has to be an expert in quality improvement but all staff and team members should understand the principles.

Sasha Karakusevic replied that getting that right can be incredibly tricky, requiring persistence and continuity.
This discussion corresponds with a theme from the evaluation of the School for Change Agents 2019. A significant number of frontline NHS staff who perceive themselves to be change agents and who have self selected to join the school regard the deployment of QI skills as a “top-down QI strategy” that stimulates negative experiences for people seeking to make change in the NHS.

Sarah Sheikha commented that she uses Whatsapp and Facebook to keep connectivity between teams.

Creating conditions for improvement


Similarly, UCLH improvement stated that staff must be given the time and space to work face to face across their normal boundaries on shared problems with a common approach.
In order to create conditions for improvement, a skill needed according to Jonathan Cliffe is courage, to start the ball rolling. He said that confidence is instilled by encouragement passed down. Senior staff encouraging junior staff, management team encourage staff groups.

In addition to Jonathan's point, James Mountford added that attitudes of the teams are vital to creating conditions for change, for example if something does not work well instead of using words like "failure" we can use "fail again, fail better.
Lynnette Lee agreed with James' point, explaining that failures are just opportunities to make things even better, the best inventions did not work on its first try.
In her own experience, Sarah Sheikh shared that blame culture is a significant barrier to change. Developing skills and the culture to accept change would improve the quality of care and improve the systems.

Compassionate leadership is required, appreciate how hard staff work to deliver care to patients said Helen. This was followed by Justine Smith who said cared for staff must equal caring staff. To watch an interesting webinar on building a culture of gratitude - click here.
Adding to the conversation, Farzana Hussain said that a learning culture needs to be promoted so staff do not feel to blame for situations.
Adding to this Dann Gooding said that three things we must focus on is improving on that blame culture, empowering others rather than putting them down and being open to change.
Lou Waters made the point that too much effort should not be invested in those who do not want to change. Invest the time and energy in those with interest.
In response, Freddie Johansson expressed that we cannot dismiss resistance to quickly either, as hidden knowledge can emerge and new relationships formed.
On a similar theme, Christopher Tuckett expressed that it's not just about encouraging people to learn, it's about developing staff members who actively seek out learning. Knowledge seeking mindset needs to be appreciated and valued. In response Matthew Mezey recommended the book 'An Everyone Culture'.
Co-production with patients

This was reinforced by Christopher Tuckett who explained that reaching and involving patients who are current or very recent service users in a truly meaningful way is a skill. Co-production rather than collaboration or consultation, which could be incredibly valuable.
Similar to Jonathan's ideas, Julia Holding said that we should do something to support health systems learn from the fantastic co-production where staff are forging partnerships with patients and carers.

Leadership
Leeanne said that as QI leaders its our responsibility to ensure healthcare professionals are given proper QI training to allow them to apply this.

In comparison, Farzana Hussain thought distributed leadership would be beneficial, a step back from the positional leader.
This was supported by Rebecca Barrett who shared that her teams have shared governance where 80 groups of nurses are actively seeking improvement and working across role boundaries.
Similarly, Alison Day shared how her team works to use the QI tools they have learnt everyday so it becomes a habit.
UCLH Improvement said that they believe building improvement capability at all levels, taking every opportunity for personal and leadership development.
There also must be the ability to see and appreciate different perspectives, said Alison Kirk.

In response, Suzie Bailey shared the Developing People Improving Care framework, brought together with the hope that CEOs will have leading improvement knowledge and skills.
Hugh McCaughey pointed out that it is visible when different organisations and teams have undergone the same training and developed the same skills, but the right leadership is vital for he embedding of those skills.

Replying to Hugh, Christopher Tuckett said much effort is placed on the 'heroic' leader to give direction, research shows that the followers have the true power.
With a similar idea, David Wells stated that a key leadership skill would be to trust and inspire the team. In his own experience, this has lead to instrumental improvement change that was championed.
Measurement for improvement
Lynette Lee said though data is important sometimes we have pages and pages of data when only some data will show a story.
Using more strengths based methodologies rather than deficit based & being brave to stop something that is not working well was shared by Lyn Williams

Tools created to aid improvement
Justine Smith shared tool cards created to support quality improvement. To access the tool cards, click here. For quick animations of often used tools, click here.

Lynnette Lee highly recommended the QI Hikers for quality improvement mini-courses. For more information about the interactive learning platform, click here.


Participating in the programme for the second time, Lyn Williams said she loves the course, recommending it to peers.

Leeanne Lockley shared her favourite tools; process map, measurement for improvement, PDSA cycle and driver diagrams.


Supported by Justine Smith who said the Q community is her way of connecting with others and learning from them, plus the support the Academic Health Science Network for the North East and North Cumbria.

The Worcestershire Health and Care NHS Trust has proposed a QI improvement framework with one of themes being building capacity and capability, shared by Elizabeth Parkes.


Similarly, Kate Slater highlighted the importance of values and shared purpose as first steps.
Thank you to everyone who joined in the tweet chat. We hope you will join us for the third #Improve4Patients tweet chat, which will be held on 31 July at 2019. The topic will be "What is the potential for quality improvement in health and care in England?"




/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-04-14-15-27-52-040-62583d78f636e9115805b2d5.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-08-05-09-59-36-465-62ecea08f636e906acfed639.jpg)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-28-14-57-17-405-62e2a3cdf636e9180c9835cb.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-20-10-16-56-533-62d7d618f636ea07987f6668.png)
/Passle/5a5c5fb12a1ea2042466f05f/MediaLibrary/Images/6168334917af5b10f4bf1d30/2022-07-15-09-55-32-858-62d13994f636ea1398e71aa9.jpg)